Abstract
Introduction
Thrombocytosis is a common presentation seen by hematologists. Within the appropriate clinical context, driver mutations of JAK2, CALR and MPL are diagnostic of a myeloproliferative neoplasm (MPN). In patients who are triple negative for these mutations, there is a diagnostic challenge when associated with isolated thrombocytosis and no clinical cause. The World Health Organization (WHO) MPN diagnostic criteria for essential thrombocythaemia (ET) and prefibrotic myelofibrosis (preMF) relies heavily on bone marrow histology despite the subjective reporting nature of this test in patients with triple-negative thrombocytosis (TNT). The WHO criteria also include the presence of a non-driver mutation (NDM) to support the diagnosis of an MPN, although the causality with an MPN diagnosis is unclear due to possible clonal hematopoiesis. The aim of this analysis was to compare the clinical and laboratory characteristics and outcomes of patients with TNT and driver mutation thrombocytosis (DMT), namely ET and preMF, in the real world setting.
Method
We retrospectively analyzed the clinical phenotype, laboratory parameters and outcome measures of TN thrombocytosis (TNT) patients with DMT patients at Aneurin Bevan University Health Board, United Kingdom. All patients had platelets >450 x 109/L in isolation, sustained on 2 occasions within 12 months, and normal blood smear morphology, no evidence of BCR-ABL1 mutation, and no obvious reactive cause. When performed, a next-generation sequencing (NGS) myeloid panel was performed using Illumina TruSight Myeloid technology on blood samples. Variables were compared using univariate analysis.
Results
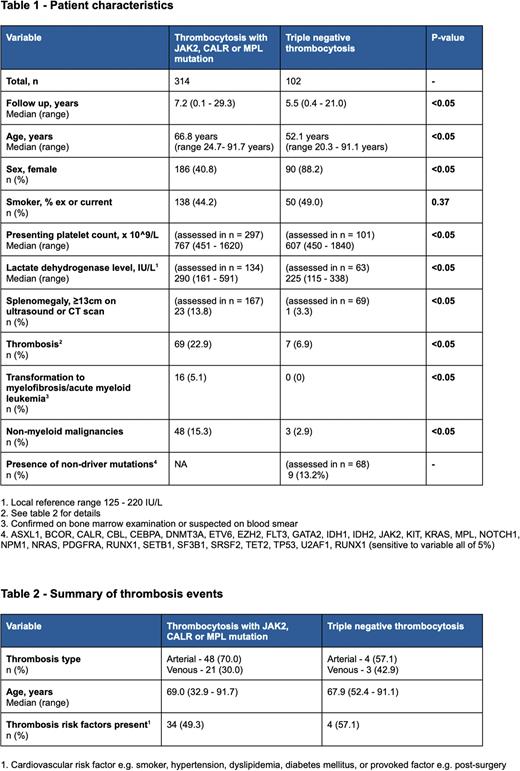
416 patients were analyzed with the data summarized in tables 1 and 2. We found distinct differences in the two groups, with TNT patients being younger (median 52.1 yr vs 66.8 yr), showing a female predominance (88.2% vs 40.8%), lower presenting platelet counts (median 607 x 109/L vs 767 x 109/L), lower lactate dehydrogenase levels (225 IU/L vs 290 IU/L), and a lower incidence of splenomegaly, defined as a spleen size >≥13cm on ultrasound or computerized tomography imaging (3.3% vs 13.8%). We also found a significantly increased incidence of non-haematological malignancies in the DMT group (15.3% vs 2.0%).
Importantly, the risk of thrombosis (7.4% vs 15.3%) and myelofibrosis/leukemic transformation (0% vs 5.1%) was significantly lower in TNT patients, although follow-up was shorter in this group (median 5.5 yr vs 7.2 years). No thrombosis occurred in TNT patients not receiving antiplatelet/anticoagulation therapy (n=66). Cytoreductive therapy was given to 14 TNT patients (Hydroxycarbamide, n=12; Pegasys, n=1,; Anagrelide, n=1) dictated by physician choice.
In evaluable patients with TNT (n=69), NDM was found in only 9 patients (13.2%) and associated with older age (median age 69.3 yr). Single mutations were seen in 8/9 patients, commonly associated with clonal hematopoiesis of indeterminate potential (CHIP) (DNMT3A, n=4; SF3B1, n=2; ASXL1, n=1; TET2, n=1). One TNT patient was found to have a TET2 and ASXL mutation, presenting with significant myocardial infarction.
Discussion
Despite the limitations of our study, e.g. retrospective nature, lack of bone marrow histology, and differences in follow-up, we identified TNT patients, generally, to have a distinct clinical phenotype (young, female, lower platelet count and LDH level, absence of splenomegaly) with a low rate of thrombosis and malignancy. We also question the importance of testing for non-driver mutations in younger TNT patients < 60 years old due to their low incidence and potential association with CHIP in older TNT patients. We hence favour the term idiopathic thrombocytosis in selected for patients with TNT patients. Further studies are warranted to examine the role of cytoreduction and anti-platelet therapy in TNT in selected patient groups, e.g. previous thrombosis , cardiovascular risk factors, older age and extreme thrombocytosis.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal